ABOUT
Hemorrhoid banding is a simple and painless procedure lasting under three minutes. It is chiefly effective in decreasing, (but not eliminating) hemorrhoid bleeding.
The procedure is usually coupled with some other examination of the colon, either colonoscopy (examination of the entire large bowel) or “flexible sigmoidoscopy” (examination of the last 30 cm only). Although the procedure is effective in decreasing bleeding, the effects are neither curative, nor permanent. Most patients can expect a decrease in bleeding by 50% or more, lasting up to two years.
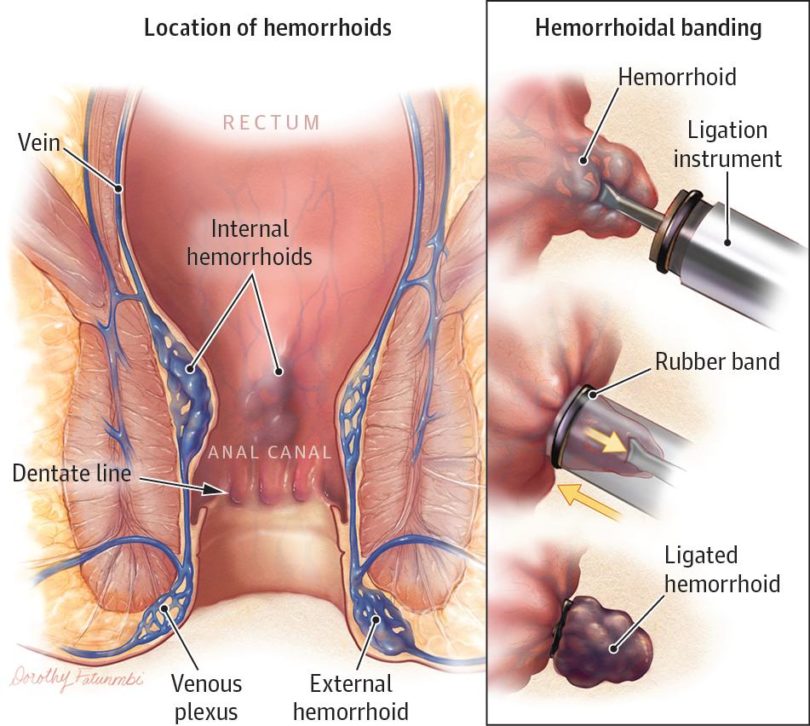
Hemorrhoids are essentially varicose veins of the anus. They cannot be individually counted, just as you cannot give an exact number to the number of veins on the back of your hand; they are all interconnected. The bands are small elastics that clip the hemorrhoid veins, causing thrombosis (clotting). The bands fall off on their own within a few days. As these clotted veins are absorbed by your body, the hemorrhoids decrease in number, and bleeding decreases. Most patients will see a slight increase in bleeding for the first few days after the procedure only.
Because the lining of the rectum cannot sense pinching or trauma, the procedure is not uncomfortable. Hemorrhoid banding does not require sedation, and does not require the same bowel preparation as colonoscopy. At Durham EndoSurgery Centre, it is typically performed at the end of the day. It can easily be done in a short, 15 minute visit. You can walk in from your car, undergo the procedure, and drive home about 45 minutes later.
You should be able to drive immediately, and fine for work the following day. Although the procedure is not uncomfortable, many patients do experience a mild sensation of ‘needing to have a bowel movement’ that lasts for several hours after the procedure, or a very mild, persistent dull, pelvic cramp which has been compared to a mild menstrual cramp. Both of these symptoms are caused by the pinching of the rectal lining, and disappear within a few hours.
The procedure is usually coupled with some other examination of the colon, either colonoscopy (examination of the entire large bowel) or “flexible sigmoidoscopy” (examination of the last 30 cm only). Although the procedure is effective in decreasing bleeding, the effects are neither curative, nor permanent. Most patients can expect a decrease in bleeding by 50% or more, lasting up to two years.
Hemorrhoids are essentially varicose veins of the anus. They cannot be individually counted, just as you cannot give an exact number to the number of veins on the back of your hand; they are all interconnected. The bands are small elastics that clip the hemorrhoid veins, causing thrombosis (clotting). The bands fall off on their own within a few days. As these clotted veins are absorbed by your body, the hemorrhoids decrease in number, and bleeding decreases. Most patients will see a slight increase in bleeding for the first few days after the procedure only.
Because the lining of the rectum cannot sense pinching or trauma, the procedure is not uncomfortable. Hemorrhoid banding does not require sedation, and does not require the same bowel preparation as colonoscopy. At Durham EndoSurgery Centre, it is typically performed at the end of the day. It can easily be done in a short, 15 minute visit. You can walk in from your car, undergo the procedure, and drive home about 45 minutes later.
You should be able to drive immediately, and fine for work the following day. Although the procedure is not uncomfortable, many patients do experience a mild sensation of ‘needing to have a bowel movement’ that lasts for several hours after the procedure, or a very mild, persistent dull, pelvic cramp which has been compared to a mild menstrual cramp. Both of these symptoms are caused by the pinching of the rectal lining, and disappear within a few hours.
SHOULD I CONSIDER BANDING?
Many patients consider banding because their hemorrhoids are causing them difficult symptoms; but it's important to state that hemorrhoid banding will only improve certain symptoms. These are bleeding, and to a much lesser extent, prolapse (the feeling of hemorrhoids protruding after a bowel movement).
If effective, banding can reduce bleeding by approximately 50%, and the improvement might last 6 - 24 months (the time it takes your body to create new, oversized hemorrhoid veins from ones that were previously normal). To notice a difference, patients will typically be experiencing bleeding on a regular basis, at least 1-2 times per week. Patients who can routinely have weeks or months between episodes of bleeding will seldom benefit from banding, as the improvements will be too small to notice.
Patients who have prolapse (the sensation of hemorrhoids protruding after a bowel movement) benefit less from banding. If the hemorrhoids (and not just the skin overlying the hemorrhoids, which is different) are outside at all times, then typically the only longterm solution is surgery. For patients who experience prolapse only after a bowel movement, the placement of bands may induce some inflammation that can reduce the amount of prolapse.
For patients experiencing raw, itchy perianal skin, the treatment is often centred around the skin itself, rather than the hemorrhoids inside. Banding hemorrhoids up inside the rectum does nothing to improve irritated perianal skin.
Finally, patients who experiencing outright pain with a bowel movement should not undergo banding. These patients are frequently suffering from an anal fissure, and banding will only make this much worse. The time to reassess whether or not the bands have been effective in decreasing your bleeding, will be about four weeks after the procedure.
Sometimes hemorrhoid banding is done as part of a strategy to confirm that infrequent rectal bleeding is in fact from hemorrhoids only. Hemorrhoid bands will not affect bleeding from cancers, colitis, or polyps. The assumption is that after the placement of the hemorrhoid bands, it will be possible a month or two later to confirm that there has been a sustained, significant decrease in the rectal bleeding. If this is the case, it goes a long way to proving that any bleeding is hemorrhoidal in nature. By the same token, rectal bleeding that is entirely unaffected by hemorrhoid bands always needs to be thoroughly investigated. Patients who have no significant response to hemorrhoid banding must follow up with their doctor.
The worst possible complication of haemorrhoid banding is infection, which is extremely rare. Any patient undergoing banding who is having increasing pain in the first week after banding should be reassessed by their doctor.
Overall, hemorrhoid banding is a useful way to treat the bleeding of moderate to severe hemorrhoids, without having to undergo more painful and invasive procedures like surgery.
If effective, banding can reduce bleeding by approximately 50%, and the improvement might last 6 - 24 months (the time it takes your body to create new, oversized hemorrhoid veins from ones that were previously normal). To notice a difference, patients will typically be experiencing bleeding on a regular basis, at least 1-2 times per week. Patients who can routinely have weeks or months between episodes of bleeding will seldom benefit from banding, as the improvements will be too small to notice.
Patients who have prolapse (the sensation of hemorrhoids protruding after a bowel movement) benefit less from banding. If the hemorrhoids (and not just the skin overlying the hemorrhoids, which is different) are outside at all times, then typically the only longterm solution is surgery. For patients who experience prolapse only after a bowel movement, the placement of bands may induce some inflammation that can reduce the amount of prolapse.
For patients experiencing raw, itchy perianal skin, the treatment is often centred around the skin itself, rather than the hemorrhoids inside. Banding hemorrhoids up inside the rectum does nothing to improve irritated perianal skin.
Finally, patients who experiencing outright pain with a bowel movement should not undergo banding. These patients are frequently suffering from an anal fissure, and banding will only make this much worse. The time to reassess whether or not the bands have been effective in decreasing your bleeding, will be about four weeks after the procedure.
Sometimes hemorrhoid banding is done as part of a strategy to confirm that infrequent rectal bleeding is in fact from hemorrhoids only. Hemorrhoid bands will not affect bleeding from cancers, colitis, or polyps. The assumption is that after the placement of the hemorrhoid bands, it will be possible a month or two later to confirm that there has been a sustained, significant decrease in the rectal bleeding. If this is the case, it goes a long way to proving that any bleeding is hemorrhoidal in nature. By the same token, rectal bleeding that is entirely unaffected by hemorrhoid bands always needs to be thoroughly investigated. Patients who have no significant response to hemorrhoid banding must follow up with their doctor.
The worst possible complication of haemorrhoid banding is infection, which is extremely rare. Any patient undergoing banding who is having increasing pain in the first week after banding should be reassessed by their doctor.
Overall, hemorrhoid banding is a useful way to treat the bleeding of moderate to severe hemorrhoids, without having to undergo more painful and invasive procedures like surgery.
LONGTERM BENEFITS?
There are no long term benefits of hemorrhoid banding. It is simply a convenient way to improve hemorrhoid bleeding, and a slightly less successful way to decrease the symptoms of prolapsing hemorrhoids, without the need for surgery.
The natural history of hemorrhoids is that they will slowly (over decades) get larger, and cause more symptoms. A small percentage of patients will run out of options and proceed to surgery. However, the large majority of patients can improve their symptoms by avoiding trauma to the perianal skin (over-wiping, scrubbing in the shower, scratching an itch), by avoiding constipation (stool softeners like fibre) and by limiting the time they spend sitting on the toilet. Simply sitting on the toilet causes the veins to become more distended, become larger, prolapse more, and bleed more. Limiting time on the toilet may be the single most important thing patients can do themselves to minimize hemorrhoid bleeding and proplapse.
The natural history of hemorrhoids is that they will slowly (over decades) get larger, and cause more symptoms. A small percentage of patients will run out of options and proceed to surgery. However, the large majority of patients can improve their symptoms by avoiding trauma to the perianal skin (over-wiping, scrubbing in the shower, scratching an itch), by avoiding constipation (stool softeners like fibre) and by limiting the time they spend sitting on the toilet. Simply sitting on the toilet causes the veins to become more distended, become larger, prolapse more, and bleed more. Limiting time on the toilet may be the single most important thing patients can do themselves to minimize hemorrhoid bleeding and proplapse.